What is the Rural Health Transformation Program?
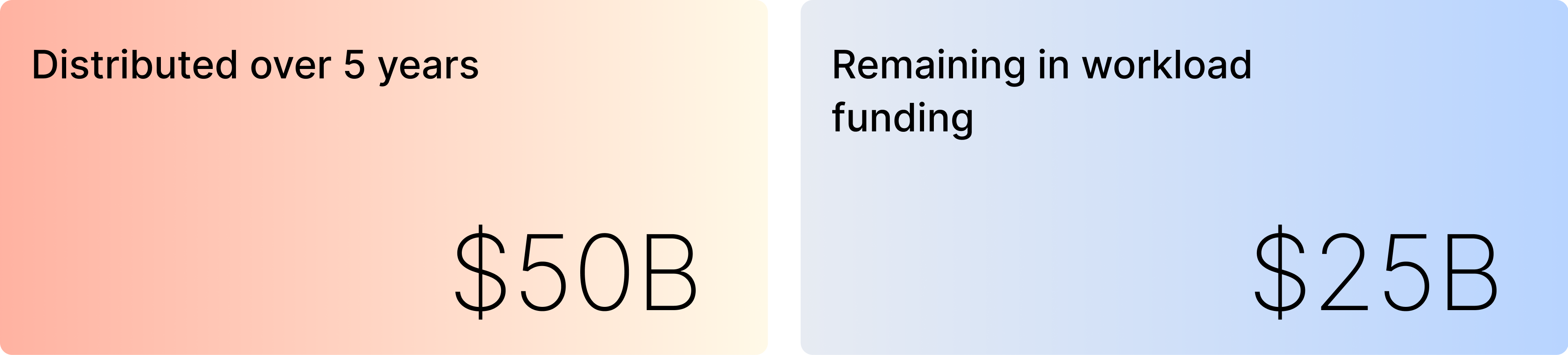
The CMS Rural Health Transformation Program (RHTP) offers a historic opportunity for states to modernize how rural residents access and experience care. With $50 billion distributed over five years, the program is designed to expand access, improve outcomes, and strengthen the long-term sustainability of rural health systems.
RHTP directly addresses the challenges rural communities face today: provider shortages, geographic barriers, fragmented care delivery, and rising costs driven by reactive models of care. Now that the initial base funding has been awarded, states must implement high-performance remote care models to maximize their share of the remaining $25B Workload Funding. The challenge for states is execution: delivering scalable, patient-centered solutions that meet RHTP population, facility, and technical requirements while producing measurable results.
Why Fabric Is the Right Partner for RHTP
Successfully executing RHTP requires a partner that can operate at statewide scale, support regional coordination, and extend the capacity of already-stretched rural providers.
Fabric is a national leader in virtual care and the Digital Front Door®, combining a comprehensive care access platform, a statewide provider directory, a 50-state clinical network, and integrated services across virtual urgent care, primary care, specialty care, and behavioral health.

By blending AI-enabled automation with synchronous and asynchronous virtual care, Fabric helps states:
- Extend the capacity of the existing rural workforce by automating intake, triage, documentation, and follow-up
- Reduce avoidable emergency department utilization through virtual urgent care
- Lower total cost of care by shifting services to lower-cost, virtual-first settings
- Enable proactive, evidence-based care in place of reactive models
- Remove geographic barriers by enabling care on any device
Fabric’s technology pioneered the Digital Front Door® concept and remains focused on a single mission: ensuring patients receive the right care at the right time, regardless of geographic proximity, while expanding provider capacity and delivering care more efficiently.
How Fabric Delivers Statewide Rural Health Transformation
Fabric turns RHTP funding into durable digital infrastructure through three core capabilities:
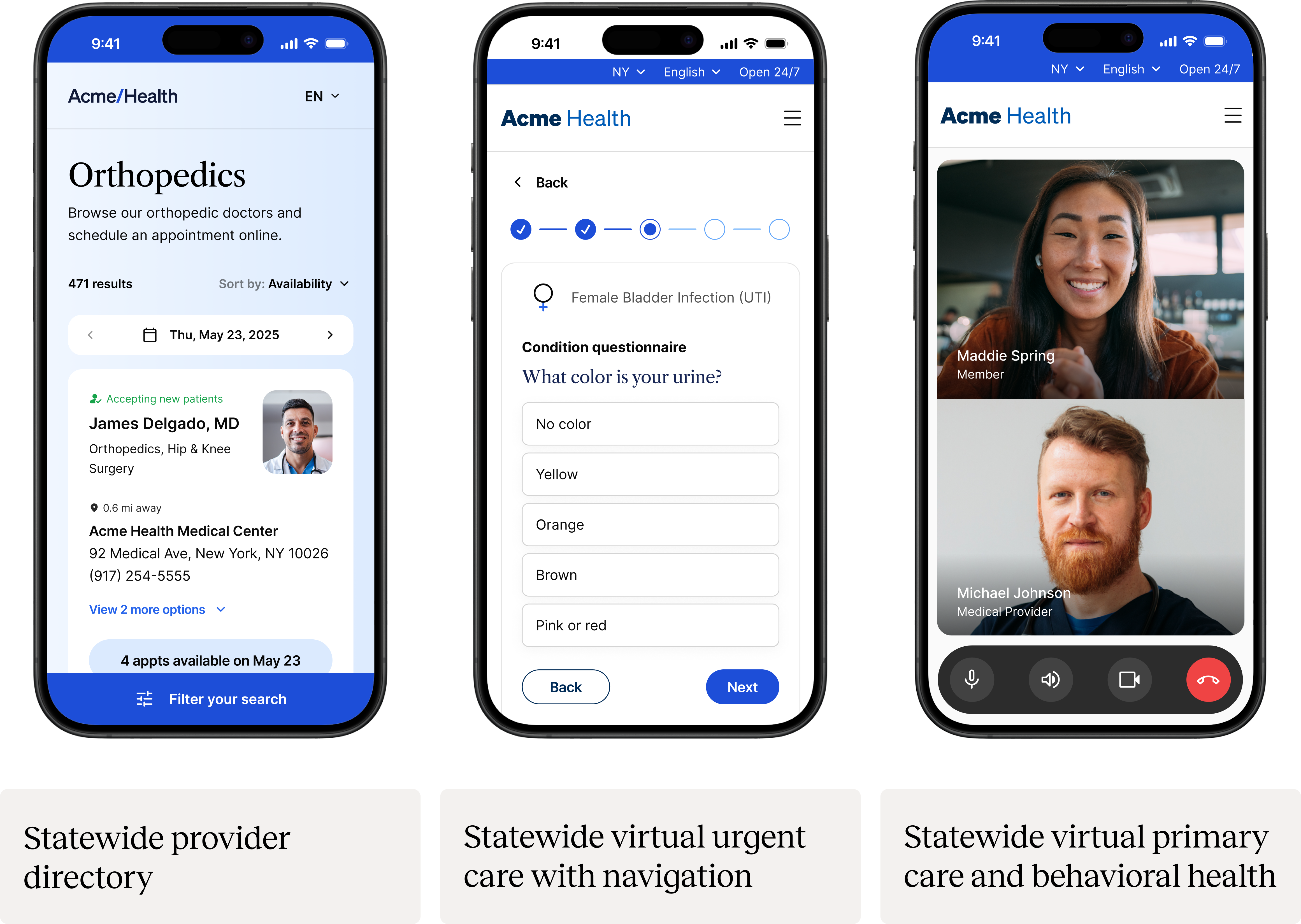
Statewide provider directory: Fabric’s statewide provider directory serves as the digital hub that powers RHTP's required hub-and-spoke regional coordination, unifying all specialties into a single, continuously updated system that enables accurate booking, confident self-scheduling, and guidance to the right level of care.
Statewide virtual urgent care with navigation: On-demand virtual urgent care paired with intelligent routing to in-person or community-based care when needed. An asynchronous-first model directs patients to the appropriate level of care while lowering costs and reducing clinical burden.
Statewide virtual primary care and behavioral health: longitudinal virtual care for underserved populations, with navigation and automated follow-up.
Together, these capabilities create a single front door to care that simplifies access for patients and expands capacity for rural providers.
Driving Sustainable, Long-Term Results
With a proven track record of innovation, scalability, and measurable outcomes, Fabric serves as a turnkey technology and clinical services partner. By aligning with RHTP sustainability requirements, Fabric helps states transition from grant-dependence to long-term viability. Our platform converts unmanaged patient demand into billable virtual encounters, creating a durable revenue stream that supports the infrastructure long after the initial 5-year grant period concludes.
Fabric’s model is designed for scalability and long-term viability beyond initial RHTP funding. A blend of PMPM subscription models, Medicaid reimbursement, and shared-savings participation ensures continued financial stability. This approach supports the goal of creating a durable, adaptable health infrastructure that remains impactful without long-term grant dependency.
Expected Outcomes and Measurable Impact
Fabric Health’s statewide deployment will drive measurable improvements in access, quality, cost, and sustainability—advancing RHTP scoring priorities and CMS objectives around health equity and rural transformation. Through patient-facing digital engagement, AI-driven automation, and statewide clinical coordination, rural states can achieve meaningful gains across near-term performance metrics and long-term structural outcomes.
Access and Equity
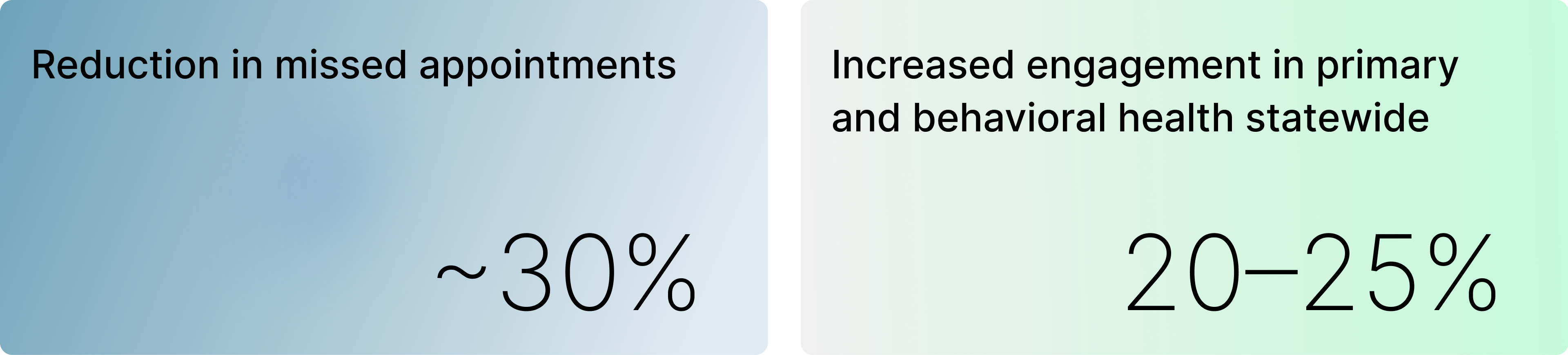
Fabric expands equitable access to care through 24/7 virtual availability, asynchronous low-bandwidth modalities, and culturally relevant care pathways. Rural residents who previously traveled long distances for basic or follow-up care gain immediate access to clinicians—improving timeliness, continuity, and satisfaction. This digital-first infrastructure is projected to reduce missed appointments by up to 30% and increase engagement in primary and behavioral health by 20–25% statewide.
- Timeliness of Care: Reduced time-to-appointment for rural residents.
- Utilization of Virtual Access: Percentage of encounters completed via telehealth, asynchronous visits, or kiosk access.
- Geographic Reach: Fewer miles traveled for routine care.
- Equity of Access: Increased participation among Medicaid, Medicare, and uninsured populations.
- Patient Satisfaction: Higher CAHPS-style scores for access, ease-of-use, and cultural responsiveness.
Clinical Outcomes
Fabric’s condition-specific Care Pathways and automated outreach improve chronic disease management across key conditions such as diabetes, hypertension, COPD, CHF, and behavioral health. Across comparable implementations, organizations have achieved measurable improvements, including reductions in readmissions, higher medication adherence, and meaningful gains in HbA1c and blood pressure control. Embedded analytics enable organizations to monitor performance at the provider, regional, and population levels.
- Chronic Disease Control: Improved HbA1c and blood pressure control rates.
- Readmission Reduction: Fewer 30-day readmissions for COPD, CHF, and maternal complications.
- Behavioral Health Engagement: Increased follow-up and treatment completion.
- Preventive Care: Improved postpartum follow-up, screenings, and vaccination rates.
Operational Efficiency and Workforce Impact
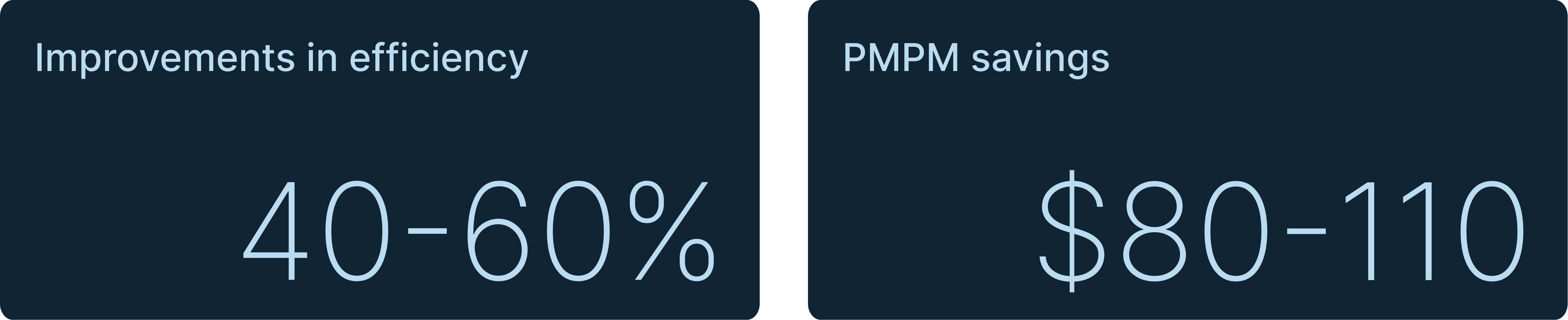
Automated outreach, reminders, and self-scheduling significantly reduce administrative burden, allowing staff to focus on clinical priorities. Fabric clients typically achieve 40–60% improvements in efficiency, equating to thousands of hours saved annually across rural networks. AI triage and asynchronous models further expand clinician capacity, enabling larger patient panels without compromising care quality.
- Provider Efficiency: Increased panel size per clinician through digital workflows.
- Workforce Satisfaction: Improved retention and reduced burnout.
- Training Uptake: Number of rural clinicians trained and using the platform.
Cost Reduction and Financial Stability
Fabric reduces unnecessary emergency visits and readmissions—the primary cost drivers in rural healthcare. Independent analyses show PMPM savings of $80-$110, largely from avoided ED utilization and improved coordination. These efficiencies strengthen financial stability for Rural Health Clinics, FQHCs, and CAHs, supporting long-term sustainability under value-based care models.
- Avoidable ED Visits: Fewer visits for ambulatory-sensitive conditions.
- Length of Stay: Shorter inpatient stays through better coordination.
- Total Cost of Care: Reduced PMPM costs via fewer readmissions and duplicative services.
- Return on Investment: Savings reinvested into workforce and infrastructure.
Data Infrastructure and Continuous Improvement
All engagement, clinical, and utilization data integrate directly into DPHHS’s analytic ecosystem for real-time tracking and evaluation. This enables performance measurement across RHTP scoring categories while ensuring accountability and continuous improvement. Statewide dashboards provide actionable insights for policymakers, providers, and communities to guide ongoing program evolution.
Operational Capacity
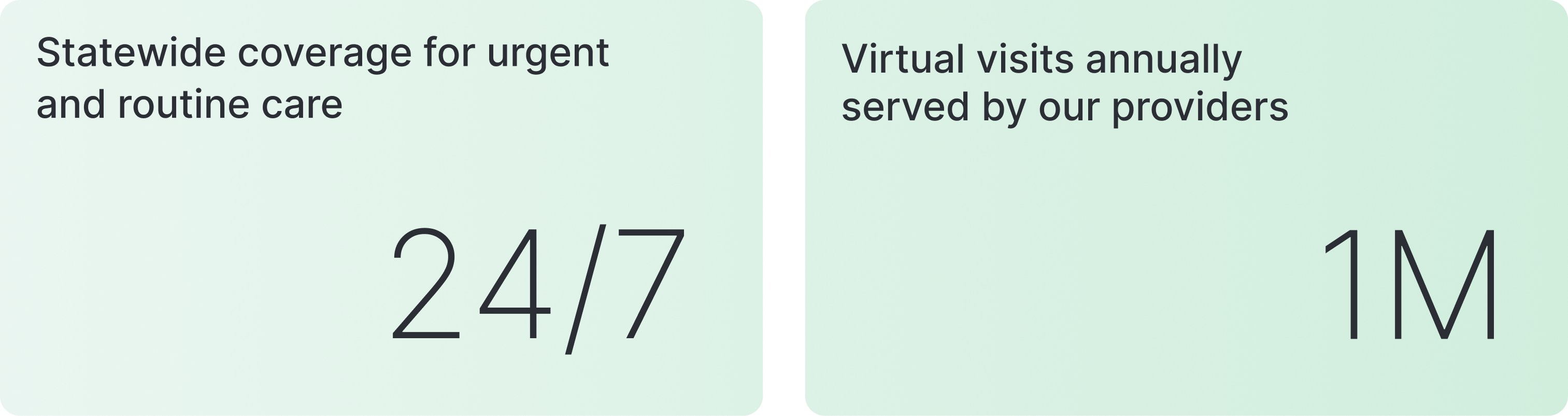
Fabric employs more than 250 dedicated staff, including engineers, client success managers, and care coordinators, who provide the operational backbone for deploying and scaling digital health solutions. In addition, Fabric maintains a nationwide network of contracted clinicians who collectively deliver and support more than 1 million virtual visits per year. These clinical resources allow us to augment provider staffing in several critical ways:
- Backstop Support: Offering overflow capacity when local providers face staffing or demand constraints.
- 24/7 Coverage: Ensuring continuous access to urgent and routine care for residents statewide.
- Mobility of Care: Supporting rural patients while traveling outside the state.
- Scalable Infrastructure: Deploying proven systems and protocols that can rapidly expand across rural communities.
This combination of dedicated staff and a national clinical network uniquely positions Fabric to advance the RHTP’s goals of expanding access, improving outcomes, and strengthening long-term rural health capacity.
Let’s Put the RHTP Into Action
Fabric partners with states to turn RHTP funding into durable, statewide care delivery infrastructure that expands access, extends workforce capacity, and ensures long-term sustainability beyond the grant period. If your team is focused on executing RHTP requirements, operationalizing hub-and-spoke coordination, and delivering measurable outcomes across rural communities, we’re ready to help.
Reach out to explore how Fabric can support your RHTP strategy and execution.