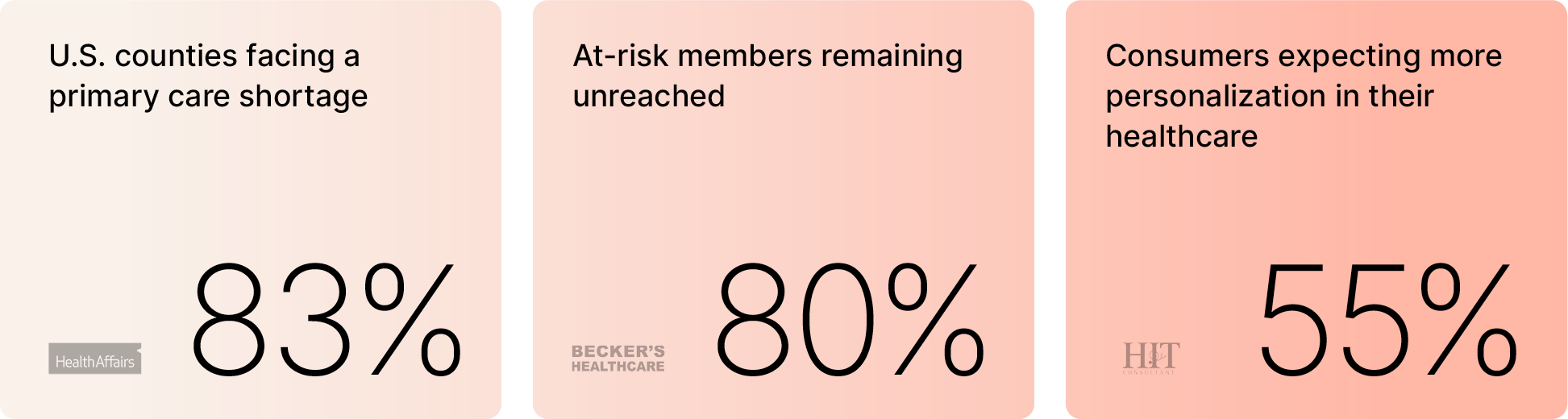
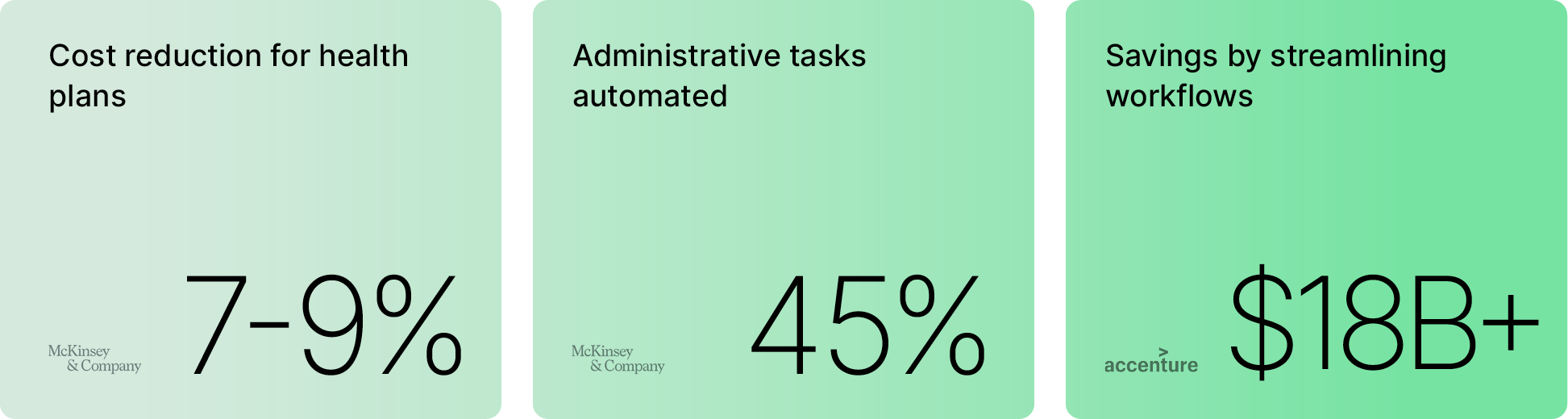
Today, nearly half of Americans struggle to afford basic healthcare, and patients wait an average of 38 days to see a doctor. At the same time, 80% of at-risk members remain unreachable. These barriers are unsustainable for members and health plans alike.
While value-based care has shifted the focus from volume to outcomes, the care delivery system has yet to fully catch up. Additionally, healthcare today faces limitations on nearly every front—from clinical capacity to patient reach.
Unmatched Potential: How AI Complements Health Plans
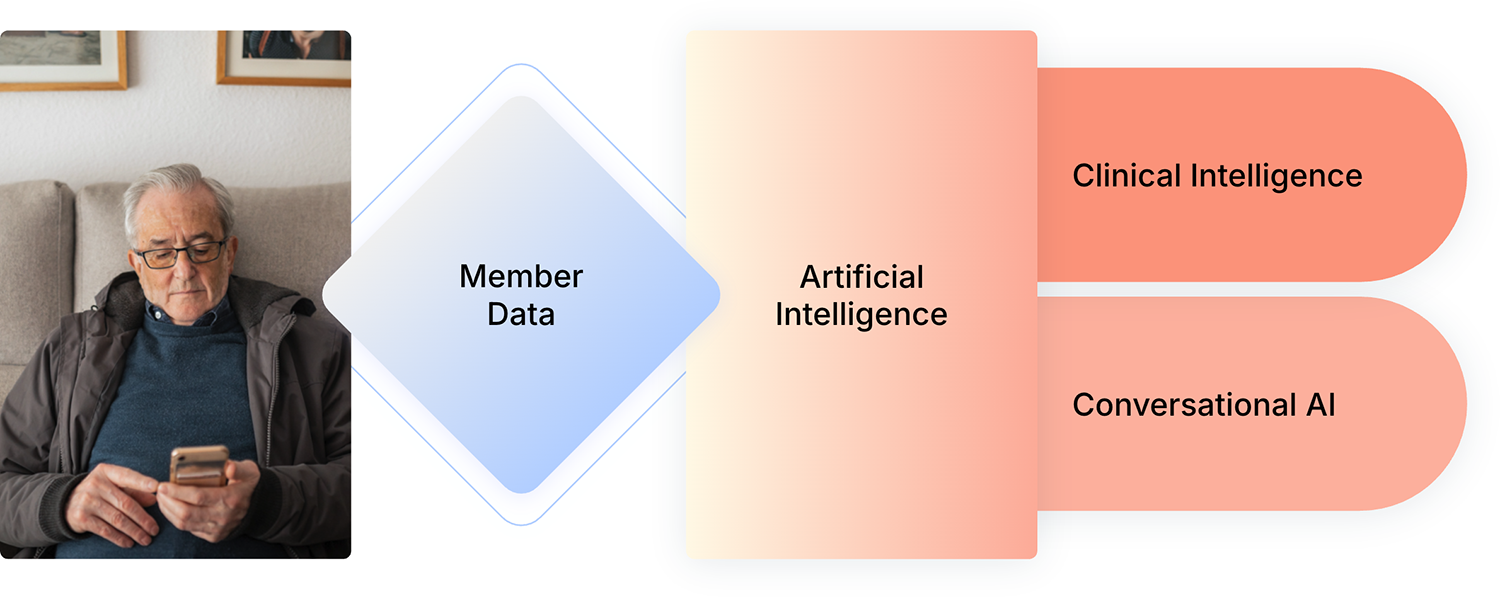
Artificial intelligence is poised to fundamentally change the economics of care delivery. It’s not about replacing care providers or automating away relationships. It’s about augmenting what’s already known with intelligent systems that reduce the cost of care.
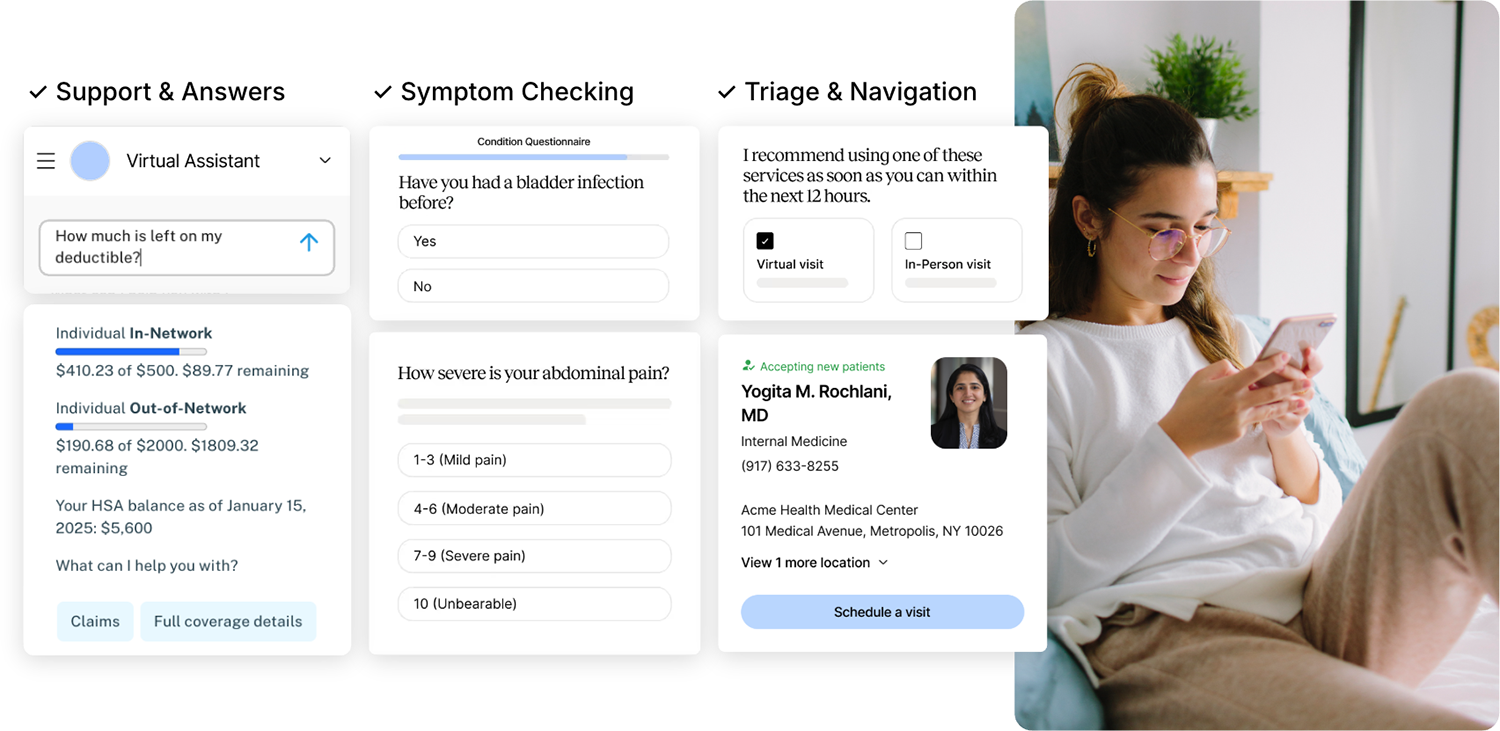
Even the most advanced AI is only part of the equation. Health plans hold rich member data that remains underleveraged. The true power lies in the intersection of AI and human insight—when health plans combine the member data and information they already have with technology that can scale personalized outreach, triage, and care navigation.
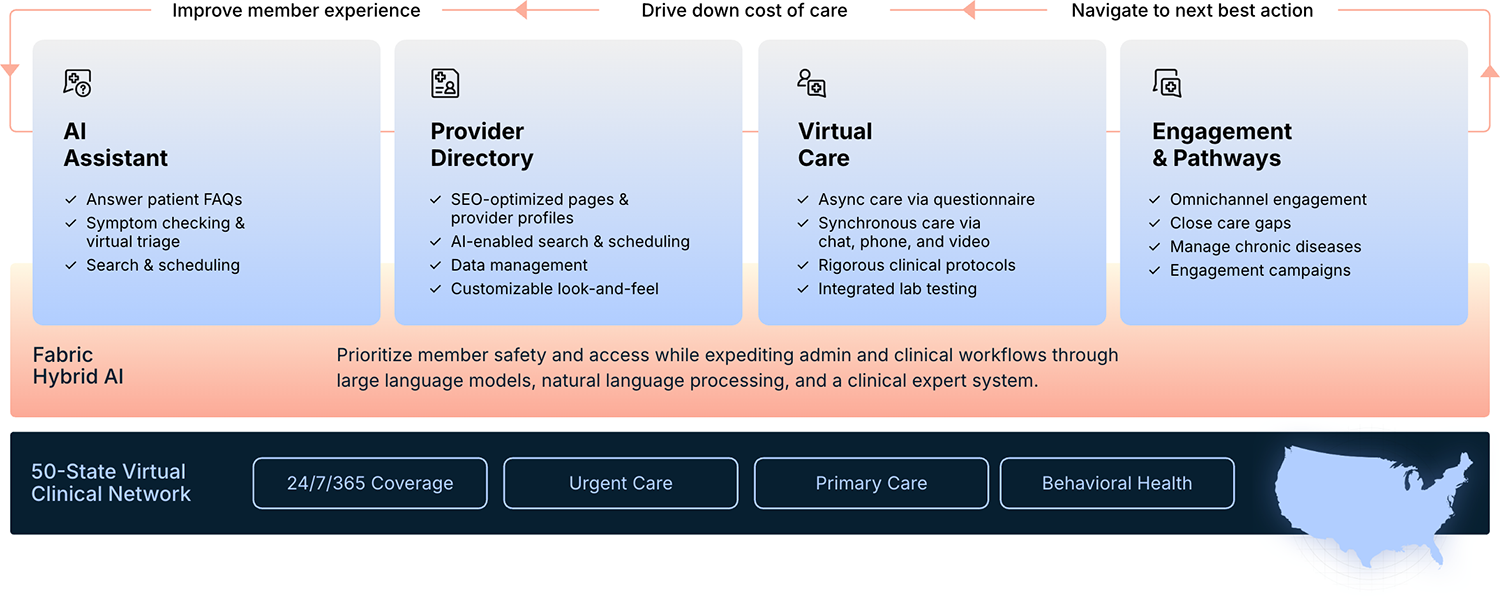
Creating Sustainable and Scalable Omnichannel Access
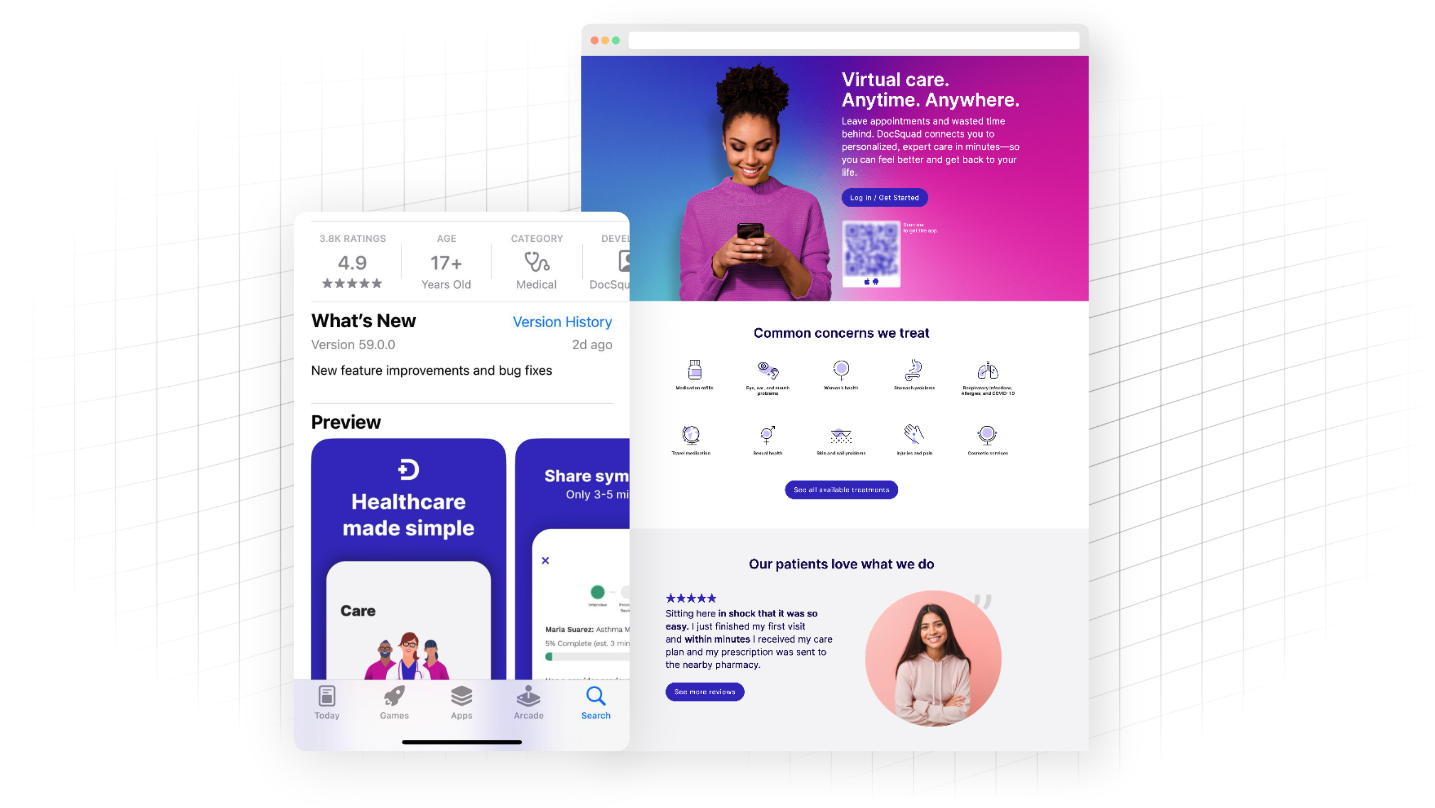
Expanding access doesn’t mean adding more apps or portals. It means meeting members where they are—on the phone, online, or at home—and routing them to the right care, in the right setting, at the right time.
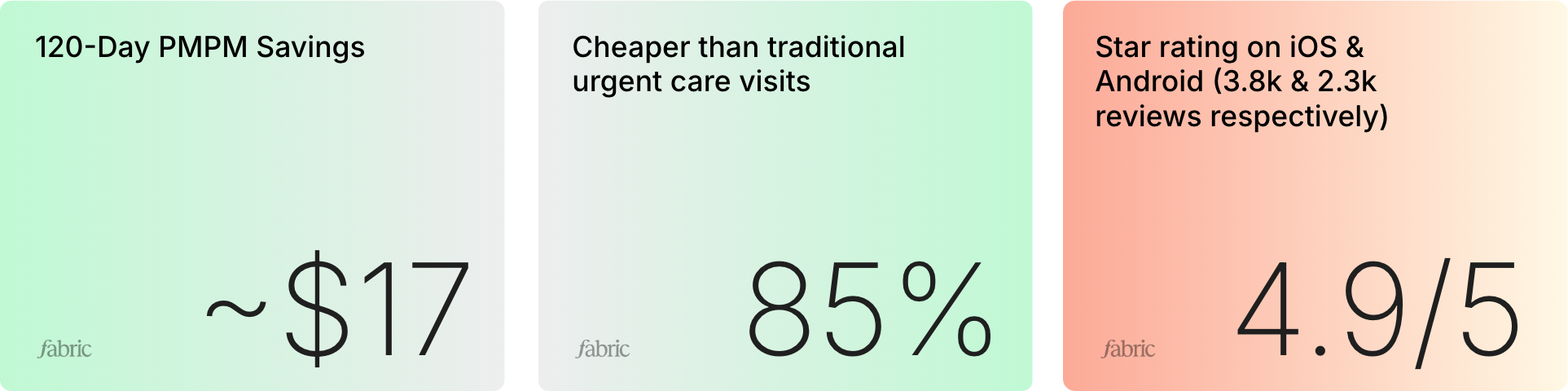
With AI-driven asynchronous-first solutions, plans can offer 24/7 access to personalized, convenient, and cost-effective care. One health plan saw $17 PMPM savings in just 120 days after implementing asynchronous-first care. Meanwhile, readmissions dropped, and satisfaction rose.
Improving Outcomes with Automated Engagement
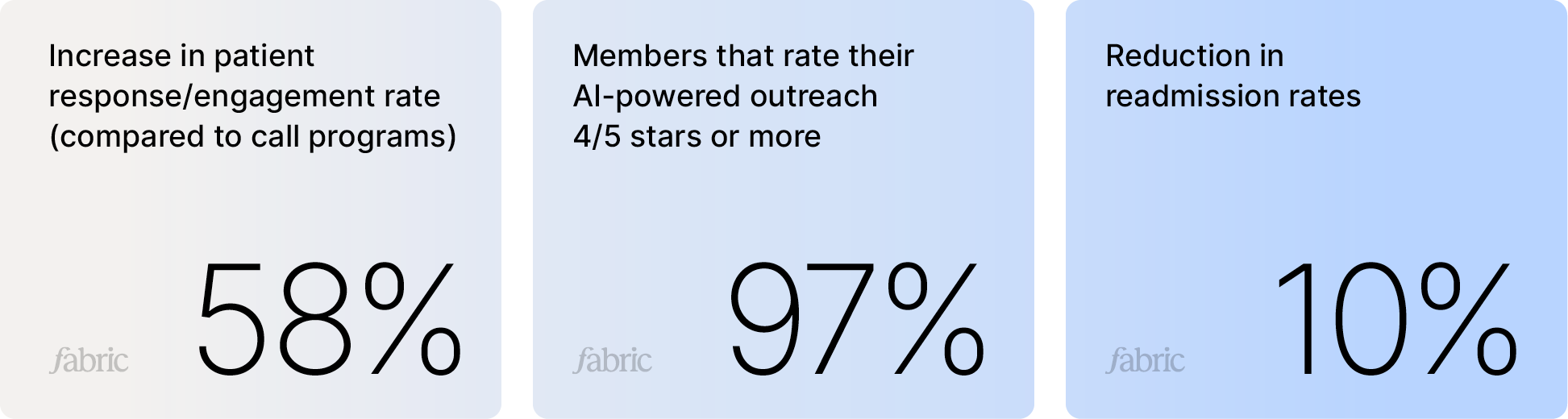
In addition to improving the way patients access care, AI also keeps patients engaged throughout their journey. From medication reminders to post-visit follow-ups, AI-driven outreach can improve adherence and reduce readmissions.
These systems outperform manual outreach efforts, driving higher response rates and better outcomes without increasing clinical burden.
The Case for More Connected Care
Unifying the care journey and streamlining workflows is not only beneficial for improving experiences but also for enhancing overall efficiency. It directly correlates to cost reduction by automating busywork to drive better efficiency. In adopting an end-to-end system, health plans can unify access, navigation, and engagement across every member touchpoint.
This is how we unlock better outcomes, stronger engagement, and lower costs—by reimagining the member experience, not just digitizing pieces of it.
The future of care isn’t piecemeal. It’s connected, personalized, proactive, and always within reach.